SPRING has drawn from various definitions of scale-up in development-related literature to draft a definition that captures its key elements. This proposed definition is intended to lay out the main principles that SPRING believes are essential for effective, wide-scale nutrition program implementation, as well as a starting point for discussions on how to measure the effectiveness of scale-up efforts, short of impact assessment.
This is a working paper to inform and serve as a basis of conversation. As SPRING continues its scale-up-related work, this definition may be updated.
Introduction

Recent years have seen the proliferation of evidence on strategies for combating malnutrition, and with it a call to action to implement these interventions on a broad scale. The Lancet’s Maternal and Child Undernutrition Series in 2008, for example, called for 99 percent coverage of eight core interventions for children and pregnant women in countries with high burdens of undernutrition (Bhutta et al. 2008); the 2013 update of the series recommended ten interventions at 90 percent coverage (Bhutta et al. 2013). Moreover, a number of initiatives have been launched to assist the scale-up of such nutrition strategies, including the Scaling Up Nutrition (SUN) Movement. Currently 50 countries have signed on to the core SUN principle of multisectoral commitment to increasing coverage of nutrition-improving interventions (SUN 2014).
This nascent movement presents an exciting opportunity for high-level nutrition advocates, program implementers, and policymakers; at the same time, examples of scaling up a unified strategy to effectively combat malnutrition are rare, and it is unclear what exactly the scaling-up process should take into account. Because of this, there is a need to define scale-up not merely in terms of expanding intervention coverage, but also the dimensions needed to achieve that coverage. SPRING has drawn from various definitions of scale-up in the development literature1 to draft a definition that can capture key elements in scale-up. This proposed definition is intended to lay out the key principles SPRING believes are essential for effective, wide-scale nutrition program implementation, as well as a starting point for discussions on how to measure the effectiveness of scale-up efforts, short of impact assessment..
Definition of Scale-Up (Proposed)
A process of expanding nutrition interventions with proven efficacy to more people over a wider geographic area that maintains high levels of quality, equity, and sustainability through multisectoral involvement.
The characteristics included in SPRING’s definition are mentioned frequently in other definitions of scale-up in the health, agriculture, and economic development sectors. Reaching more people over a wider geographic area is mentioned in almost all definitions. Table 1 summarizes the results of the literature review, showing select scale-up characteristics that are mentioned by each definition. In developing its understanding of scale-up, the SPRING project highlighted characteristics in two categories: components and types of scale-up.
Components of Scale-Up

This proposed definition lays out key principles for effective, wide-scale nutrition program implementation, as well as a measurement of the effectiveness of scale-up efforts. We provide a rationale and an explanation of select components below that we consider essential to defining and measuring scale-up efforts.:
- Proven efficacy: The majority of the definitions found in the literature included the requirement that the planned interventions demonstrate real improvements at a smaller scale. However, several documents explicitly acknowledged that the evidence base for scaling up was under-controlled, experimental, or otherwise relatively homogenous populations and that successful scale-up would entail more than mere replication (CORE Group 2005; Victora et al. 2004; Linn 2012; Milat et al. 2012; WHO and ExpandNet 2009; Hartmann and Linn 2008; Hodgins 2013). Similarly, The Lancet’s series selected nutrition-sensitive and -specific interventions based on studies in discrete areas of the world, yet acknowledged the gap between trial effectiveness and scaled-up effectiveness by modifying the interventions’ delivery platform according to context (Bhutta et al. 2013). This characteristic provides a rationale for scaling up, but mere replication is likely not enough. More research is needed to determine the drivers of successful scale-up and inform translation from pilot to large-scale programming.
- Quality: Three documents, all products of field experiences with scaling up health activities, named quality as a defining characteristic. The CORE Group highlighted quality both of implementation and of the end benefits to the target group. Victora and colleagues note the importance of focusing on quality because in practice, trade-offs between it and coverage are often made. This aspect is applicable to nutrition programming in particular because it often requires raising demand for services (such as antenatal care) or changing behaviors ingrained in social norms or environmental realities (such as infant and young child feeding), which are not likely to change with poorly-implemented interventions.
- Equity: Much like other areas of health and development, those most in need of nutrition interventions are likely the poorest and hardest to reach in each country. By simply aiming for a certain level of coverage, the most disadvantaged might still be missed in scale-up efforts (CORE Group 2004). Victora and colleagues note that accounting for equity should also affect the very design of the intervention, such as the selection of delivery platforms or the decision on whether to build up the capacity of existing ones (such as immunization days).
- Sustainability: Several sources mentioned the need to ensure continued and sustained commitment when scaling programs up. The underlying assumption is that programs in need of scale-up generally cannot achieve their long-term development goals without continued and concerted efforts. The emphasis on sustainability may also be a reaction to several actual scale-up efforts, which failed to secure resources in the long term due to issues like vertical funding and programming, waning commitment and shifting priorities, and lack of planning (CORE Group 2005; Victora et al. 2004; Hartmann and Linn 2008). To sustain scaled-up programs requires “vertical” scale-up, or institutionalization of required changes at multiple levels of the relevant system (CORE Group; WHO and ExpandNet) from national to local, in order to achieve “horizontal” scale-up (expanding coverage across people and space) (Hartmann and Linn 2008). Some sources also noted the need for country ownership—including both decision making and financial independence—in order to achieve sustainability (CORE Group; Hartmann and Linn 2008).
Types of Scale-Up

Aside from the components described above, SPRING also identified three different types of scale-up discussed in the literature. These types can be implemented separately or jointly, depending on need and circumstance. However, effective and sustainable scale-up of programming will likely require all three types of scale-up, which include:
- Horizontal scale-up: Menter et al. (2004) describes horizontal scaling up as a process that “implies adapting knowledge and innovations to the conditions of different end-users,” a process which requires “training and support networks” for on-the-ground implementers. This idea of scale-up as an expansion of coverage and/or programming to new end-users plays a prominent role in all definitions of scale-up, as can be clearly seen in Table 1, where every definition contains a reference to increased or expanded coverage of services. Horizontal scale-up is important because it expands coverage of an intervention to a wider number of people.
- Vertical scale-up: The discussion of scale-up by Menter et al. (2004) defines vertical scale-up as an “institutional” process, which broadens the stakeholders and sectors involved in the intervention from the local to national or even global levels. In the process of vertical scale-up decision-making moves from the individual to collective levels or from simple to complex organizations, and institutions internalize the program or project principles. Vertical scale-up is important to ensure buy-in by local actors and support program sustainability.
- Functional scale-up: Hartmann and Linn describe this type of scale-up, which moves beyond one function (e.g., health and education) to include others. Although they write that this factor is optional to the scale-up process, they also note that ignoring it could pose “a serious threat to the long-term success of development interventions.” They provide the example of vertical funding for specific diseases that ignore the cross-cutting weaknesses of health systems overall, and contrast it with PROGRESA, a conditional cash transfer program to improve public service utilization across the health and education sectors to improve nutrition. Functional scale-up improves quality and sustainability of programs and allows for expansion of the program through different platforms.

Concurrent with Hartmann and Linn’s example and the SUN Movement’s emphasis, SPRING believes that multisectoral involvement is especially salient for nutrition program scale-up and impact. Though multisectoral is not a component that is widely discussed in the literature, SPRING felt its important role in functional scale-up necessitated its inclusion into the draft definition with the other key components.
It is important to note that although these requirements of scale-up are presented individually, in reality they are closely interconnected and dependent on one another. Maintaining high-quality services and programming in underserved areas, for example, is essential for promoting equitable outcomes in nutrition. Moreover, individual programmatic decisions, such as selecting delivery mechanisms and developing financial plans, impact several of these areas at once. Finally, these features of effective scale-up likely share similar enabling factors, such as strong country leadership and managerial capacity and robust monitoring and evaluation systems. Figure 1 lays out the components and types of scale-up described above.
Figure 1. Scale-Up Conceptual Framework
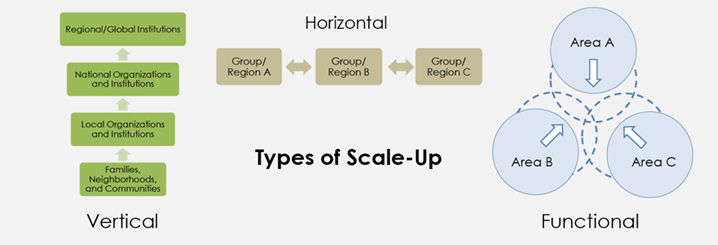
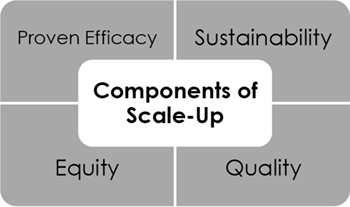
Table 1. Definitions of Scale-Up in the Development Literature, and Included Characteristics
| Source/Year | Definition | Proven Efficacy | Quality | Equity | Sustainability |
|---|---|---|---|---|---|
| CORE Group 2005 | “…efforts to bring more quality benefits to more people over a wider geographic coverage area more quickly, more equitably and more lastingly.” | x | x | x | x |
| Victora et al. 2004 | “A policy that builds on one or more interventions with known effectiveness and combines them into programmatic delivery strategy designed to reach, high, sustained and equitable coverage at adequate levels of quality in all who need interventions.” | x | x | x | x |
| Linn (IFPRI) 2012 | Expands, replicates, adapts, and sustains successful policies, programs, or projects to reach a greater number of people | x | x | ||
| Mangham and Hanson 2009 | Increasing the coverage of health interventions (extending the geographic reach such that it benefits a greater number of people) or increasing the financial, human, or capital resources required to expand coverage | ||||
| Milat 2012 | (Scalability) The ability of a health intervention shown to be efficacious on a small scale and or under controlled conditions to be expanded under real world conditions to reach a greater proportion of the eligible (target) population, while retaining effectiveness | x | |||
| WHO and ExpandNet 2009 | Deliberate efforts to increase the impact of health service innovations successfully tested in pilot or experimental projects so as to benefit more people and to foster policy and program development on a lasting basis. | x | x | ||
| Hartmann and Linn (Brookings Institution) 2008 | The expansion, replication, adaptation, and sustaining of successful policies and programs in space and over time to reach a greater number of people | x | x | ||
| Hodgins (MCHIP) 2013 (draft) | Increased quality and population coverage (and equity) of current interventions/services on a sustained/sustainable basis; and adoption, expansion, and sustained achievements of high population coverage of new high-impact interventions | x | x | x | x |
| Adamou (MEASURE Evaluation) 2012 (draft) | [A process with] two key elements: institutionalizing the practice (obtaining buy-in from leaders and stakeholders that translate into legal, political, and institutional changes) and expanding/replicating it (moving from one geographic area to more areas or one health service level) | x |
Footnotes
1 A supporting literature review was conducted for articles in the published and gray literature focused on defining scale-up. The review included searches in Google, Google Scholar, and PubMed using the following key words: scale OR scaling AND up; plus one of the following: nutrition, health, agriculture, development. Documents that did not explicitly define scale-up and devote significant space to explaining the definition were cut due to the large number of resulting articles on scale-up generally. In addition, two projects highly experienced in scale-up of programs in the health sector, MEASURE Evaluation and MCHIP, were included.
References
Adamou, Brigit. 2012. Guide for Monitoring Scale Up of Health Practices and Interventions (DRAFT). MEASURE Evaluation PRH.
Bhutta, Zulfiqar A, Tahmeed Ahmed, Robert E Black, Simon Cousens, Kathryn Dewey, Elsa Giugliani, Batool A Haider, et al. 2008. “What Works? Interventions for Maternal and Child Undernutrition and Survival.” The Lancet 371 (9610): 417–40. doi:10.1016/S0140-6736(07)61693-6.
Bhutta, Zulfiqar A, Jai K Das, Arjumand Rizvi, Michelle F Gaffey, Neff Walker, Susan Horton, Patrick Webb, Anna Lartey, and Robert E Black. 2013. “Evidence-Based Interventions for Improvement of Maternal and Child Nutrition: What Can Be Done and at What Cost?” The Lancet 382 (9890): 452–77.
CORE Group. 2005. ‘Scale’ and ‘Scaling-Up’: A CORE Group Background Paper on "Scaling-Up Maternal, Newborn, and Child Health Services (link is external).
Hartmann, Arntraud, and Johannes Linn. 2008. Scaling Up: A Framework and Lessons for Development Effectiveness from Literature and Practice. Wolfensohn Center for Development Working Paper 5. Washington, D.C.: Brookings Global Economy and Development.
Hodgins, Steve. 2013. “Draft Guidance on Scale-Up”. Draft. Washington, DC: Maternal and Child Health Integrated Program (MCHIP).
Linn, Johannes F., ed. 2012. “Scaling Up in Agriculture, Rural Development, and Nutrition (link is external).” International Food Policy Research Institute.
Mangham, Lindsay J., and Kara Hanson. 2010. “Scaling up in International Health: What Are the Key Issues?” Health Policy and Planning 25 (2) (March 1): 85–96. doi:10.1093/heapol/czp066.
Milat, A. J., L. King, A. E. Bauman, and S. Redman. 2012. “The Concept of Scalability: Increasing the Scale and Potential Adoption of Health Promotion Interventions into Policy and Practice.” Health Promotion International (January 12). doi:10.1093/heapro/dar097.
Menter, Harriet, Susan Kaaria, Nancy Johnson, and Jacqueline Ashby. 2004. “Chapter 1: Scaling Up.” In Scaling Up and Out: Achieving Widespread Impact through Agricultural Research, edited by Douglas Pachico and Sam Fujisaka, 9–24. CIAT.
Scaling Up Nutrition. 2014. “SUN Countries - Scaling Up Nutrition.” Accessed April 11.
Victora, Cesar G, Kara Hanson, Jennifer Bryce, and J Patrick Vaughan. “Achieving Universal Coverage with Health Interventions.” The Lancet 364, no. 9444 (October 2004): 1541–48. doi:10.1016/S0140-6736(04)17279-6.
World Health Organization (WHO) and ExpandNet. 2009. Practical Guidance for Scaling Up Health Service Innovations (link is external). Geneva: WHO.