
In June 2014, SPRING/Bangladesh conducted a tippy tap and handwashing study in 120 households in the Khulna and Barisal divisions of Bangladesh: we included 61 households with a female member who had recently graduated from the nine-month SPRING Farmer Nutrition School (FNS) and 59 households with similar characteristics to FNS participant households but that were not affiliated with the project. These 59 households served as a comparison group (non-FNS).
Our primary objective with this study was to explore whether promotion of handwashing and tippy taps through FNS participation improved handwashing practices. We paid special attention to handwashing at critical junctures,1 such as prior to handling and preparation of food, eating or feeding a child, after using the toilet, and other key moments. We also observed the household environment, the disposal methods of animal and children’s feces, sources of water, and who among family members were more likely to wash hands. We collected data through structured observations on the homestead and structured interviews with mothers from observed households. We used in-depth interviews with key informants to gain further information on the perception and use of tippy taps and other water sources.
Our overall findings demonstrate that the presence of tippy taps in and around the household, as well as the promotion of handwashing, has a significant positive impact on handwashing practices. Not only were all FNS participants aware of tippy taps, but they also had at least one (usually two) installed in their compound. In contrast, no households in the non-FNS group had a tippy tap installed and only one person in the comparison group had even heard of them. Furthermore, household members in the FNS group washed hands more often at critical moments than did members of non-FNS households, and more often used proper techniques. Mothers who have completed handwashing education are more than twice as likely to practice proper handwashing as other FNS household members. Although FNS children demonstrated more frequent proper handwashing behavior, numbers are still very low, indicating the need to include children in proper handwashing and tippy tap promotion and activities to help convey the importance of this practice. Results from our observations clearly illustrate better practices in FNS households, with other members (i.e., not the mother) in FNS households exhibiting proper handwashing behavior in 42 percent of instances, compared to 10 percent of instances in non-FNS households. However, in interviews, mothers reported their husbands to be more accepting of the tippy tap than their mothers-in-law.
Our observers noted FNS participants washing both hands with soap and water 46 percent of the time, whereas individuals in the non-FNS group did so only 11 percent of the time. When FNS group members washed hands at critical junctures, tippy taps were used 55 percent of the time, with various other handwashing stations used 45 percent of the time.2 However, we found a notable difference between adherence to proper handwashing following contact with stool and proper handwashing prior to eating, with participants, even FNS household members, being less vigilant about washing hands prior to feeding themselves or their children. This finding contrasts with what respondents believe they should be doing, with more than 85 percent saying it is important to wash hands before eating, and 60 percent saying it is also important to wash hands before cooking and after using the latrine. We found that washing both hands with soap before three critical moments—handling food, eating, and feeding a child—was significantly more likely in the FNS groups than the non-FNS group, suggesting that a kitchen-based tippy tap does encourage improved handwashing practices.
Although we recorded notable differences in the level of knowledge and practices in the FNS group versus the non-FNS group, both knowledge and practices remain weak in many areas, including washing hands more frequently (versus sometimes) at potential critical handwashing moments. We also identified knowledge gaps in both groups, especially as regards the connection between contaminated hands and disease. Handwashing following contact with livestock is very low, approximately 20 percent for both groups.
These findings underscore the effectiveness of incorporating handwashing education and tippy tap promotion into nutrition and livelihoods programming. Participants reported tippy taps as easy to use and conveniently located, facilitating handwashing around the times when it should occur. Therefore, we recommend that any activity that aims to improve nutrition outcomes, whether through homestead food production or other activities, should promote the use of tippy taps as an affordable and accessible means of handwashing. Handwashing promotion should pay particular attention to contact with food and livestock to address the links between handwashing, environmental enteropathy, nutrition, and health. Additionally, we acknowledge that greater impact on hygiene and health is likely if broader sanitation issues are addressed in the handwashing education along with tippy tap promotion and use.
Background

Bangladesh is greatly affected by water, sanitation, and hygiene challenges. As noted by Rabbi and Dey (2013), water and sanitation–related diseases are considered some of the most significant diseases among the children of Bangladesh. As they reported, unclean water and improper sanitation practices can cause diarrhea, worm infections, cholera, malaria, trachoma, and schistosomiasis. Water-related diseases account for an estimated 24 percent of all deaths and gastroenteritis and diarrheal diseases, killing 110,000 children younger than five every year in Bangladesh (Rabbi and Dey 2013).
Numerous studies around the world provide evidence that handwashing with soap prevents infections and saves lives. Human and animal feces are the main source of pathogens that children are exposed to. These pathogens cause shigellosis, typhoid, cholera, pneumonia, and many other gastroenteric and respiratory infections. One gram of human feces may contain approximately 10 million viruses and one million bacteria (PPPHW 2013). The pathogens spread from an infected host to a new one via various routes (fecal-oral, direct physical contact, etc.). The moment a person finishes washing hands, the next cycle of collecting germs starts over by opening doors, wiping faces, playing with toys, and changing diapers. This process cannot be avoided, but the chances of infection can be greatly reduced by knowing when and how to properly wash hands (Canadian Paediatric Society 2001). Research shows that children living in households where handwashing with soap is a norm had one-half the diarrheal rates of children living in households that do not wash hands with soap (PPPHW 2013). Washing hands is easy, effective, and affordable. Integrating the habit of handwashing saves more lives than any single vaccine or medical intervention (PPPHW 2013).
Poor water quality and hygiene practices also lead to undernutrition. Globally, about 35 percent of child deaths per year are related to undernutrition (USAID 2013). The cause of undernutrition is not just lack of food. Food intake, caloric or protein deficiency, and periods of illness also contribute to stunting or chronic undernutrition. Other factors, such as maternal and child care practices, hygiene practices, and access to clean water are crucial for adequate nutrition outcomes (USAID 2013). A 2010 study conducted in Bangladesh found that handwashing with soap was much more common after defecation than before food preparation or child feeding, and that inadequate handwashing prior to food handling led to contamination of the food and increased incidence of child diarrhea (Luby et al. 2011). There is a vicious cycle of diarrheal diseases and undernutrition: children suffering from diarrhea eat less and absorb a lower proportion of nutrients from the food they consume. Consequently, these children have greater susceptibility to diarrhea when exposed to fecal material in their environment.
Recently, a connection has been noted between poor sanitation and hygiene and stunting through the subclinical condition called environmental enteric dysfunction (also known as environmental enteropathy [EE]). Solomons et al. (1993) suggested a link between impaired growth in children and increased microbial gut load, similar to that observed in chickens. Later, Humphrey (2009) hypothesized that exposure to fecal bacteria due to poor hygiene causes enteropathy. Environmental enteropathy is characterized by villous atrophy, crypt hyperplasia, increased intestinal permeability, inflammatory cell infiltrate, malabsorption, and other processes (Ngure et al. 2014). Such processes weaken absorptive and barrier functions of the small intestine mucosa lining, causing inadequate absorption of nutrients, and thus, growth failure.
Further evidence of a correlation between hygiene practices and the nutritional status of children has been shown in Bangladesh. Gracey (1996) identified malnutrition and impaired cell-mediated immunity as independent risk factors for diarrheal episodes. Whatever the complexities of the interactions between diarrhea and malnutrition, these problems undoubtedly have their greatest impact in the first three years of life and, particularly, during the second half of infancy (6–12 months) (Gracey 1996). However, too often, highly effective and inexpensive hygiene interventions are overlooked. Simple actions like handwashing with the use of tippy taps can prevent diarrhea, environmental enteropathy, and undernutrition, even in high-exposure environments.
Modifying existing handwashing practices can be challenging. While dissemination of handwashing education is important and effective, people are not likely to change behavior simply because they have received information about the health benefits of handwashing. In developing countries, people are more likely to adopt proper handwashing because of disgust, as a reason to be seen as a good parent, to appear attractive, or to protect and nurture children. Additionally, the distance between the handwashing location and the toilet facility also significantly influences handwashing behavior in developing countries. However, once individuals have adopted handwashing with soap at critical junctures, it tends to become regular practice.
The presence of handwashing stations with water and soap has been shown to increase handwashing and hygienic behaviors, resulting in a reduction in incidence of diarrheal diseases, especially in young children (icddr,b 2012) Tippy tap research in Uganda found that, in intervention areas where participants received tippy taps plus handwashing education, handwashing rates increased by more than 90 percent (Schreyer Honors College 2014). However, limited research exists on the effectiveness of the tippy tap and washing stations as a means of removing or reducing barriers to handwashing. There is also limited information on whether the presence of tippy taps encourages handwashing. Additionally, researchers to date have focused most studies on tippy tap use in Africa (Biran 2011); these studies do not address the social and cultural drivers, barriers, and behaviors specific to South Asia and, particularly, Bangladesh.
By understanding the effect of tippy taps and hygiene messages, as well as some of the behavioral determinants of handwashing at critical junctures (before eating, before handling food, after using the latrine, after cleaning a child’s bottom, and after handling livestock) (Hernandez et al. 2012), on hygiene practices, behaviors, beliefs, and attitudes, we can help determine whether or not a tippy tap installed in a household has an effect on handwashing practices.
SPRING focuses on the prevention of stunting in the first 1,000 days. In Bangladesh, SPRING promotes and supports the Essential Nutrition Actions (ENA), the Essential Hygiene Actions (EHA), and homestead food production (HFP) in 40 upazilas (subdistricts) in Barisal and Khulna divisions. We aim to strengthen the delivery of ENA and EHA at all health contacts within the health system, and combines the delivery of ENA, EHA, and HFP during the agriculture extension worker sessions and during FNS gatherings. Our FNS represents a bimonthly gathering of 20–25 pregnant and lactating women and mothers of children under two where participants learn, through practical, hands-on training, and improved HFP practices, as well as ENA and EHA practices.
In these sessions, we promote a simple water-saving technology, the tippy tap, in the context of nutrition to reduce barriers to handwashing in areas without running water. The tippy tap consists of a used plastic water bottle with an adjustable nozzle for regulating water flow that creates a simple, affordable handwashing station in any location where handwashing should occur (Annex 1). Specifically, we encourage all FNS participants to install tippy taps in two key places around the homestead: near the latrine and near the kitchen. Over a nine-month period, we provide participants in FNS with repeated ENA/EHA messaging to continually reemphasize the importance of good hygiene in the context of proper child health, nutrition, and development. Our key messages in these FNS sessions focus on the importance of handwashing during critical juncture; handwashing methods that do not require a lot of water (such as the tippy tap); the importance of handwashing after handling poultry; methods for keeping containers and food clean and why this is important; and family members who should practice essential hygiene. In addition to our repeated demonstration and message reinforcement, we also engage participants in creating self-efficacy through group work in which they build the tippy tap and prepare it for installation.
From October 2012 to September 2013, our SPRING-supported FNS promoted handwashing practices and installation of tippy taps near latrines and kitchens for more than 26,000 women in the Barisal and Khulna divisions. An informal study conducted by Helen Keller International (HKI) in October 2013 found that 100 percent of the sample of SPRING FNS participants had a tippy tap hung in or around their homes and 66 percent exhibited appropriate handwashing practices at critical junctures, compared to 30 percent and 8 percent, respectively, of the sample of non-SPRING FNS participants (Annex 2). This finding suggested a positive impact of tippy taps on handwashing practices, and indicated a need for more rigorous investigation.
Objectives and Hypothesis
The primary objective of the study was to explore whether the promotion of handwashing and tippy taps through FNS participation improved handwashing practices, especially prior to handling and preparation of food, eating, feeding a child, or after using the latrine. The study also aimed to answer the following questions:
- Does FNS participation improve handwashing practices at critical junctures and among different members of the same household, where one member (pregnant or lactating woman/mother of child under two) recently received information on handwashing and has agreed to set up a tippy tap in the household?
- Does FNS participation in conjunction with the presence of the tippy tap near the kitchen improve handwashing practices prior to handling food, eating, and feeding a child?
The following hypothesis guided this study: participants who have been exposed to handwashing promotion and received support in groups or through individual counseling are more likely to have a tippy tap in their household and to exhibit appropriate handwashing behaviors than participants who have not been exposed to handwashing promotion.
Methodology
We designed our study as a comparison study using mixed methods, including semi-structured key informant interviews, structured observations, and structured in-depth interviews to examine differences in use of tippy taps and handwashing practices between FNS participants (persons who had received handwashing education) and non-FNS participants (persons who had not received education about appropriate handwashing).
Key informant interviews provided information and critical feedback on perceptions, practices, and common beliefs about handwashing practices and use of tippy taps that could be intentionally or unintentionally concealed by study participants. Key informants differ from other participants because they are culturally specialized informants, chosen for their competence in particular areas such as medical knowledge, FNS activities, and community health concerns. In this case, the key informants included health care professionals, SPRING IPNGO (implementing partner/nongovernmental organization) staff, teachers, and other community leaders who are familiar with handwashing messaging and promotion activities in their communities, and provided essential insider vision on barriers, beliefs, and practices. We conducted five key informant interviews in total.
The SPRING project maintains lists of all women/households who met the inclusion criteria and were vetted to participate in the SPRING FNS program, including those whom we subsequently included in FNS and those we did not. Our inclusion criteria are pregnant women, lactating women, or mothers of children under two who fall into the two lowest wealth quintiles. Our total sample was randomly selected from these lists using stratified random sampling. Participants were split into two strata: recent3 FNS graduates (FNS group) and non-FNS participants (comparison group). We then randomly selected participants from each strata using a random numbers table until a total of 120 were selected (60 in each group).4 All study participants were chosen from the same districts and/or upazilas in Barisal, Patuakhali, Bhola, Khulna, and Jessore districts. In most cases, however, participants from the FNS and non-FNS groups were from the same upazila or union, but from different villages (Table 1).
Table 1. Geographic Locations of Study Participants
| Non-FNS Locations | FNS Locations | ||||
|---|---|---|---|---|---|
| District | Upazila | Village | District | Upazila | Village |
| Khulna | Terokhada | Katanga Boroitala | Khulna | Terokhada | Barasat Nachuniya Parokhali |
| Khulna | Dhigolia | Biddabagispara Goalpara Lakhohati | Khulna | Dhigolia | Barakpur maddhaya Para Goalpara Brammagati |
| Jessore | Jessore Sadar | Azmatpur Rohomotpur Dokkinpara Arenda Kalidarpara | Jessore | Jessore Sadar | Teghoria Kamarpara Barohaibatpur Labutala Dakkhin Teghoria |
| Barisal | Bakergonj | Bharpasha Dakshinkathi Runshi | Barisal | Bakergonj | Ata-khati Lakshmipasha Parshibpur Rajapur |
| Bhola | Bhola Sadar | Pascim Illsha Lamchipata Dakkhin Charpata Paschim Shibpur | Bhola | Bhola Sadar Pascim Elisha | Charpotka Kelashpura (Kalashura?) Nobipur/Guli Nobipur Pashcim Charpata |
| Patuakhali | Patuakhali Sadar | Purba Hetalia Sarikkhali Uttar Hetalia | Patuakhali | Patuakhali Sadar | Kochabaria Kochabunia Dibuapur Maderbunia |
We conducted observations and in-depth interviews with 61 FNS participants who were exposed to the handwashing promotion, and with 59 non-FNS participants who matched FNS inclusion criteria but did not participate in FNS (and, therefore, have not received handwashing promotion).
Data concerning behavioral practices, such as handwashing, are often overestimated through traditional self-reporting surveys or in-person interviews (Joint Commission 2009). To increase the potential for quality and accuracy and minimize influence on observed behaviors, we shared with participants that our study aimed to observe their daily activities and water usage, not their handwashing practices. We did not mention handwashing or tippy taps while obtaining consent. Additionally, rather than using self-reporting surveys, we used structured observations of each household included in the sample. Our data collectors observed household domestic activities for three hours and noted instances of critical junctures for handwashing, handwashing practices, locations and methods, and details concerning the handwashing stations, if there were handwashing stations present. Practices at these critical junctures were recorded. Data collectors observed daily activities not only among the mothers, but among all members of the same household. Including observations of all members of the family is important because other family members may also participate in childcare, food preparation, and so on, and can spread bacteria or viruses as well. Immediately after observations, data collectors conducted structured in-depth interviews with the study participant (i.e., the pregnant or lactating woman/mother of a child under two years old in the household) to gain insight into individual preferences, attitudes, knowledge, beliefs, and practices about handwashing and tippy taps. Each interview lasted from a half hour to an hour.
We conducted observations and interviews daily, with each data collector responsible for two households per day: one observation and interview in the morning, from approximately 7:30 a.m. to 11:30 a.m., and one observation and interview in the afternoon, from approximately 12:30 p.m. to 4:30 p.m.
Limitations
The possible limitations of this study are as follows:
- Occasionally, observed individuals seemed uncomfortable eating in the presence of a data collector. On several occasions, families waited to eat until the data collector’s departure. This limited our opportunity to observe and record activities surrounding handwashing before the preparation or consumption of food.
- The goal of our study was to gain a better understanding of the influence of handwashing education and presence of tippy taps, rather than carry out large-scale surveillance; however, the study’s probability sample represents the target population in project areas and was designed to detect large differences. Where differences are statistically significant, they can be extrapolated to the population beyond the sample.
- Our study is not a pre-/post-design; therefore, we cannot say whether behaviors have improved among the intervention group, relative to the comparison group. The difference can be observed only after implementation. There is a chance, however unlikely for some of the behaviors, that the differences observed may predate the intervention.
Findings from Observation
Respondent Profile
We collected data from a total of 120 households during a two-week period in the first half of June 2014:
- 61 FNS participants (recent FNS graduates)
- 59 non-FNS participants (comparaison group)
We included equal numbers of participants from the two administrative divisions, Khulna and Barisal, where we implement SPRING activities. Within each division, equal numbers of FNS and non-FNS households participated in the study. As a whole, the FNS and non-FNS groups had similar demographics, as shown in Table 2.
Table 2. Demographics of Observed Households
| Respondents | Mother's Age | Family Size | Household Income Level (Monthly, in Bangladeshi taka [BDT]) | Mother’s Education Level Completed | Religion | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Avg. | Range | Avg. | Range | Mode | Range | Mode | Range | Percentage | ||
| All (n=120) | 24.9 | 15-35 | 5.3 | 2-10 | 5K-7K | Less than 3K – more than 10K | Primary | Non-literate - higher education | 96% Muslim 4% Hindu | |
| FNS participants (n=61) | 25.5 | 17-36 | 5.4 | 2-10 | Primary | Non-literate - secondary XII | 98% Muslim 2% Hindu | |||
| Non-FNS participants (n=59) | 24.3 | 15-36 | 5.2 | 3-10 | Primary | Non-literate - higher education | 93% Muslim 7% Hindu | |||
All households in the FNS group had children at the time of the observation. In the non-FNS group, 55 (93 percent) households had children, while the remaining households had women who were pregnant at the time of the observation, but no other children. Of 120 households in total, 80 percent (n=96) had children 24 months of age or younger (48 in each group). Among FNS group households, four had two children two years of age or younger, either from the same mother or from different family members living under the same roof. Most households in both groups had multiple children of different ages.
Household Environment
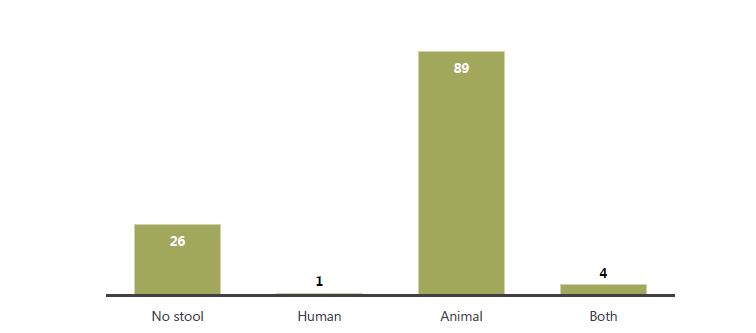
Our data collectors assessed the home compound environment for cleanliness and the presence of feces, both human and animal. The majority (n=94, 78 percent) of all households had stool in the yard. We found no significant difference between FNS and non-FNS households, although a slightly higher percentage of non-FNS than FNS households had feces in the yard (83 percent and 74 percent, respectively). Animal stool (cow, poultry, goat) in the compound was the most common type of stool (93 of 94 households, 99 percent), with human stool observed in the yards of five households (4 percent). Of those five households, four had both human and animal stool in the yard (Figure 1). Of the 93 households with animal stool, 67 percent (n=62) had one type of animal stool, 24 percent (n=22) had two types of animal stool, and 10 percent (n=9) had three types of animal stool visible in the yard.
Figure 1. Type of stool observed in yard for total sample
In 61 households (51 percent), our observers recorded 67 instances of children defecating. In 35 of those cases (more than one-half, at 52 percent), the children defecated on the ground (open defecation), while a plastic child’s training potty was used in five cases, and a latrine was used seven times. We found no significant difference between FNS (31 percent, n=19) and non-FNS (29 percent, n=17) households in open defecation by children. The remaining instances were defecation on someone holding the child (n=6), on a cloth/paper (n=12), other (n=4), and the observer did not know (n=1). Although Bangladesh has made great strides in reducing open defecation, HKI/Bangladesh has found in previous work that, frequently, children’s waste is not viewed as dirty or contaminated and may not be considered when reporting defecation in relation to potential contamination. Additionally, it is common for young children who are old enough to walk, but not yet potty trained, to wear short, loose pants. These children are not yet accustomed to using the latrine or potty and may not pull the pants down to defecate in the yard, increasing the chance of spreading the stool if defecation occurs in the pants. In all but one of the 35 instances of observed child open defecation, the stool was removed from the yard and disposed of elsewhere, almost always in the trees or bushes surrounding the homestead (69 percent of cases for FNS, n=9; 93 percent of cases for non-FNS, n=14). More FNS households disposed of stool sanitarily than non-FNS households, primarily in the latrine (n=3 for FNS and n=1 for non-FNS), although the numbers are too low to be significant. In one FNS case, the feces were thrown in a pond.
Given the expansive presence of animal stool in the yard, the opportunity for oral-fecal contamination was high. In 62 households (35 from FNS and 27 from non-FNS), we observed children under two touching the ground and then their mouths an average of 1.9 times during the three-hour observation period (range of 0–9). However, less than one-half (37 percent) of small children from those 62 households had their hands washed by an adult during the observation period. More frequent ground and mouth touching was not associated with washing hands. In fact, 23 children observed touching the ground and their mouths were also observed having their hands washed, whereas 39 children who touched the ground and their mouths did not have their hands washed during the three-hour observation period. However, more than three times as many FNS participant households (n=18, or 51 percent) whose children touched the ground and their mouths washed their children’s hands than non-FNS households (n=5, or 19 percent). Furthermore, although we found no significant difference in the presence of stool in the yard between groups, twice as many FNS households with stool present washed their children’s hands than non-FNS households. These findings provide further support for including handwashing promotion in nutrition programming, as the risk of developing environmental enteropathy could be elevated for people who have animal or human feces in their yards. Because a higher microbial gut load has the potential to negate the benefits of optimal nutritional intake, proper handwashing is essential to improving nutrition outcomes, especially for young children who habitually put their hands in or near their mouths.
Source of Water to Wash Hands
In the interviews, we asked participants about the source of water they use for various daily household activities, as well as for washing hands (Table 3). The most popular source of water for both groups was tubewell water, especially for drinking, cooking and washing food, washing children, and washing hands. Tubewell water was also more frequently used than water from other sources for washing other household items and for bathing. Although respondents sometimes used pond water for cooking and even drinking, they used it more often for cleaning activities, such as cleaning the home and washing clothes. We found no significant difference in usage of water sources for daily chores between the two groups. However, we did find a significant difference in usage of water sources between geographic locations, with participants in Khulna division using tubewell water while participants in Barisal show near equal use of tubewell and pond water. Indeed, 97 percent (n=58) of respondents in Khulna division report using tubewell water for washing hands, while 3 percent (n=2) report using pond water. In contrast, 63 percent (n=38) of respondents in Barisal division include tubewell water as a source for washing hands and 52 percent (n=31) of respondents cite pond water. This disparity exists for all domestic activities for which we collected data (listed in Table 3), but disappears for drinking water. Tubewell is overwhelmingly the preferred source for drinking water.
Table 3. Source of Water for Daily Activities*
| Activity | FNS Participants (n=61) | Non-FNS Participants (n=59) | ||||||
|---|---|---|---|---|---|---|---|---|
| Pond | Tubewell | Rain | River *** | Pond | Tubewell | Rain | River** | |
| Washing clothes | 25 | 42 | 2 | 2 | 29 | 35 | 2 | 2 |
| Washing hands | 14 | 53 | 3 | 2 | 19 | 44 | 1 | 2 |
| Washing body | 25 | 37 | 1 | 2 | 30 | 35 | 0 | 2 |
| Washing children | 17 | 47 | 0 | 2 | 16 | 46 | 1 | 2 |
| Cleaning home | 25 | 39 | 0 | 2 | 22 | 40 | 1 | 2 |
| Cleaning cooking pots and utensils | 25 | 45 | 0 | 2 | 22 | 41 | 1 | 2 |
| Washing food | 14 | 54 | 1 | 0 | 18 | 48 | 3 | 2 |
| Cooking food | 15**** | 57 | 6 | 2 | 2 | 46 | 12 | 2 |
| Drinking | 3 | 60 | 3 | 0 | 10 | 56 | 8 | 1 |
*Results are not exclusive. Some women were using different sources of water for the same activities.
**Respondents from Patuakhali district.
***Respondents from Barisal district.
****Of 15 FNS participants, four said that they use pond water only for cooking rice. People do not like that tubewell water containing iron turns their rice a red color.
Data collectors noted the visibility of a tubewell from the kitchen and from the latrine at each homestead (i.e., if a tubewell can be seen from these locations). In 57 percent (n=68) of total households, a tubewell was not visible from either the latrine or kitchen (Table 4). Although a slightly lower proportion of FNS households (39 percent) than non-FNS households (48 percent) had a tubewell visible, we found no difference in the proportion of FNS mothers (68 percent) and non-FNS mothers (68 percent) across the sample who were observed fetching water from a tubewell.
The relationship between geographic location and tubewells is noteworthy. The majority of participants from Khulna division had visible tubewells (n=48 visible, or 80 percent), while the majority of Barisal division participants did not (n=50 not visible, or 83 percent). This difference was statistically significant (p=.000) and is a likely explanation for fewer observations of washing children’s hands in Barisal, as well as fewer respondents in Barisal using tubewell water for handwashing and domestic activities. Furthermore, although not statistically significant (p=.07), a larger proportion of mothers were observed fetching water from any source in Khulna (n=47, 60 percent) than in Barisal (n=38, 63 percent). All of those same 47 mothers in Khulna fetched water from a tubewell, compared to 26 mothers in Barisal. Thus, a longer distance from the tubewell is associated with fewer trips to the tubewell and may be a barrier to refilling the tippy tap or other handwashing stations and, therefore, likely influences the number of times a person washes their hands or a child’s hands and may result in prioritizing critical junctures to reduce clean water consumption.
Another potential factor for lesser use of tubewell water in Barisal, apart from visibility of the tubewell, could be the high iron content. While most people prefer using tubewell water for cooking, more than 11 percent of respondents in Barisal report using treated pond or river water, especially for cooking rice. Because of the high concentration of iron in tubewell water, people report that the rice turns red during cooking, which they dislike. It could be worth exploring if high iron content is undesirable for household activities, including washing hands, and if tubewells in Barisal have higher iron content than tubewells in Khulna. It is important to note, however, that even in Barisal, where handwashing is less frequent, FNS participants are still more likely to wash their children’s hands and their own hands than non-FNS participants.
Table 4. Visibility of Tubewell from the Latrine and/or Kitchen
| Participants | Visible (Percentage of Participants Group) | Not Visible (Percentage of Participants Group) |
|---|---|---|
| FNS | 24 (39%) | 37 (61%) |
| Non-FNS | 28 (48%) | 31 (53%) |
| TOTAL | 52 (43%) | 68 (57%) |
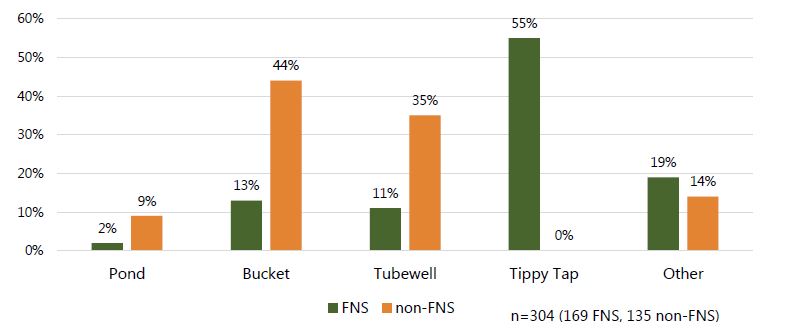
Data collectors observed 476 critical junctures, among all family members, where handwashing should have occurred.5 In total, all participants the observer was able to see washed their hands in 304 instances (169 among FNS participants and 135 among non-FNS), or 64 percent of the time (note, this is not a measure of proper handwashing, just any handwashing).6 Figure 2 shows the sources of water used by all family members to wash hands at those critical junctures. FNS household members washed their hands 68 percent of the time and non-FNS household members washed their hands 54 percent of the time. Of the 169 instances in the FNS group, 55 percent (n=93) used tippy taps. Of the 135 instances in the non-FNS group, no one used a tippy tap, with buckets (44 percent, n=60) and tubewells (35 percent, n=46) being the two most popular choices, even for proper handwashing of both hands with soap.
Figure 2. Water sources utilized during observed instances of handwashing at critical junctures among all members of the homestead7
Approximately 61 percent (n=73) of all study participants had soap available next to their preferred handwashing station. Only 10 participants (1 FNS and 9 non-FNS), or 16 percent, did not have soap present somewhere on the homestead. Data collectors noted the presence of soap inside the home, next to a handwashing station, or next to or in the latrine. Additionally, they were asked to enter the latrine after the observation period and note the presence of water and soap.
Looking at the number of tippy taps among households in the FNS group (n=61), 58 (95 percent) had two tippy taps hanging in their compound: most had one inside or near the kitchen and another one near the latrine (Table 5). These are the two places where we encourage placing the tippy tap. Of the four households that had a tippy tap in front of the house or outside the bedroom, three of them had three or more tippy taps, or one in or near the kitchen, one near the latrine, and the additional third tippy tap in front of the house or outside of the bedroom. Only one household had only a single tippy tap, which was hung on the front of the house. It is unclear why the only tippy tap in this household was not located near the latrine or kitchen. Tippy tap uptake and usage vary significantly between FNS and non-FNS groups. All recent FNS graduates had a tippy tap hung in their compound at the time of observation compared to no members of the non-FNS group. Only one woman from the comparison group knew what a tippy tap was. “I know about it because there is one (tippy tap) in my father’s house. I know how to use it, and how to make a good tippy tap,” said a non-FNS respondent. However, she did not have a Tippy Tap at her house.
Table 5. Location of Tippy Taps
| Where is a tippy tap located (n=61)? | Number of Tippy Taps |
|---|---|
| Near or inside the kitchen | 59 |
| Near the latrine | 57 |
| In front of the house/outside the bedroom | 4 |
Handwashing Practices among Mothers in Both Groups

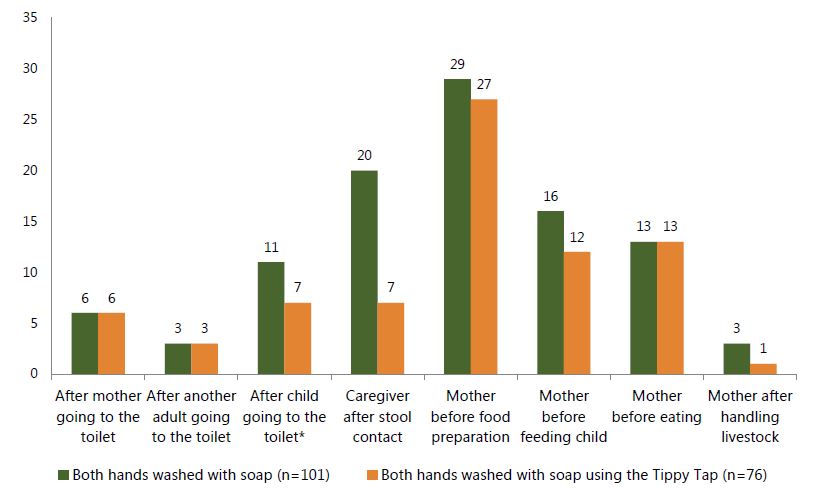
Washing both hands with soap at critical junctures, such as after using the toilet or before preparing food and feeding a child, is crucial for keeping a child healthy and preventing diarrhea and environmental enteropathy, which can lead to adverse nutritional outcomes, such as wasting (acute diarrhea) and stunting (chronic enteropathy). The rate of FNS mothers who wash both hands with soap at such moments is significantly higher than those from the non-FNS group (p less than 0.000). This is true for most of the critical junctures. For example, 24 mothers (8 from FNS participants and 16 from non-FNS) were observed going to the toilet during the observation period. Immediately after completion, nine mothers (over one-half) from the non-FNS group did not wash their hands at all, while six of the eight FNS mothers not only washed their hands, but washed them correctly (i.e., washed both hands with soap) and they chose the tippy tap near the toilet to do the washing. Only one mother of the 16 observed in the non-FNS group washed both hands with soap after using the toilet.
Table 6 displays the number and percentage of proper handwashing differences between FNS and non-FNS participants. Only in the practice of handwashing after handling livestock was there a notable difference between the two groups. We should note that these results highlight washing both hands with soap only, and do not account for other methods, such as washing both hands with water, one hand with water, or one hand with soap. When calculating the total instances of observed proper and improper handwashing, the data (not shown) revealed that at 67 percent of observed critical junctures, mothers at least attempted to wash one or both hands with water, soap, or soapy water (75 percent, n=141, of FNS observations; 60 percent, n=113, of non-FNS observations). Although non-FNS mothers did not wash their hands after using the toilet in 56 percent (n=7) of observations, one-half (n=4) of those who did attempt to clean their hands washed one hand with water only. Similarly, before food preparation, in 22 percent (n=8) of non-FNS observations, mothers did not wash hands at all, but for 57 percent (n=21) of non-FNS observations of food preparation, they used only water, usually for both hands. Thus, handwashing as a practice is not uncommon among the target population, but handwashing with soap, especially both hands with soap, is uncommon.
Table 6. Number of Times Mothers Were Observed Washing Both Hands with Soap at Critical Junctures
| FNS (n=61) | non-FNS (n=59) | P-value (Fisher’s exact test for individual rows; chi-square test for totals) | |||||
|---|---|---|---|---|---|---|---|
| Number of Observed Critical Junctures with Mothers | Number of Times Mothers Washed Both Hands with Soap | Percentage of Time Mothers Washed Both Hands with Soap at Critical Junctures | Number of Observed Critical Junctures with Mothers | Number of Times Mothers Washed Both Hands with Soap | Percentage of Time Mothers Washed Both Hands with Soap at Critical Junctures | ||
| After using toilet | 8 | 6 | 75% | 16 | 1 | 6% | 0.001 |
| After cleaning child following defecation | 16 | 10 | 63% | 24 | 6 | 25% | 0.025 |
| After disposing of child's stool* | 12 | 9 | 75% | 19 | 5 | 26% | 0.040 |
| Before food preparation | 51 | 29 | 57% | 37 | 2 | 5% | 0.000 |
| Before feeding child | 52 | 16 | 31% | 47 | 3 | 6% | 0.002 |
| Before eating | 35 | 13 | 37% | 32 | 2 | 6% | 0.003 |
| After handling livestock | 13 | 3 | 23% | 15 | 3 | 20% | 1.000 |
| Totals | 187 | 86 | 46% | 190 | 22 | 12% | 0.000 |
Handwashing Practices among All Family Members in Both Groups
Other members of the family were also included in the three-hour observation in FNS and comparison groups. Data collectors observed a total of 138 children under five years old (100 children 24 months old and younger, and 38 children 24–59 months old). Among 67 children under five who defecated during the observation period (four of them twice), 46 percent of FNS (n=13) and 21 percent of non-FNS (n=7) washed their own hands, had their hands washed, or were bathed by an adult. Both hands were washed with soap for only seven FNS children (23 percent, 31 observations) and three non-FNS children (8 percent, 36 observations). Among the seven FNS children, three used a tippy tap to wash both hands with soap. Although FNS children demonstrated more frequent proper handwashing behavior, numbers are still very low, indicating the need to include children in proper handwashing and tippy tap promotion and activities to help convey the importance of this practice.
An additional 100 school-age children (i.e., over five years of age) were observed on the homestead. Of these, only 13 used the toilet during the observation period (n=8 FNS, n=5 non-FNS). One-half (n=4) of the FNS school-age children washed both hands with soap using a tippy tap and one other used the tippy tap but without soap (data not shown). The other three either did not wash their hands or did not use soap. Only one non-FNS child used soap at all and one-half of the time the children did not wash their hands.
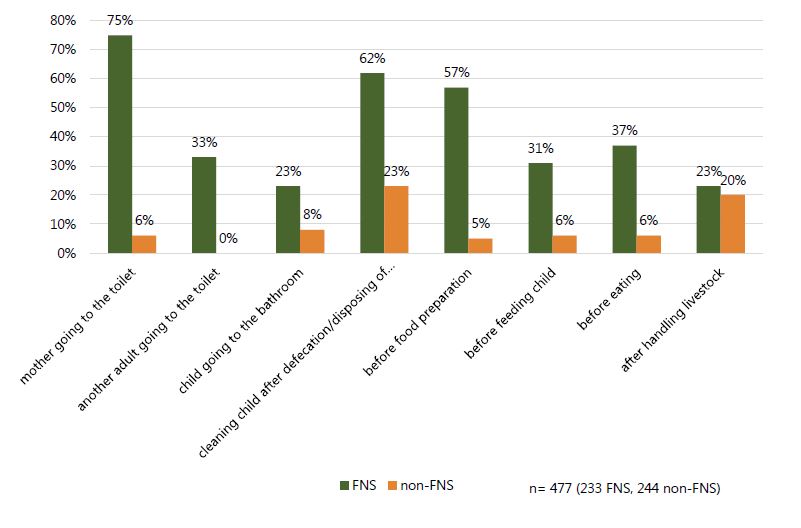
Overall, handwashing by all family members is significantly higher among FNS households than in non-FNS households (p=0.000), with proper handwashing observed 42 percent of the time in FNS households, in contrast to 10 percent of the time among members of households that have not participated in our FNS (Figure 3).
Figure 3. Number of times handwashing of both hands with soap occurred at critical junctures among ALL members of a compound
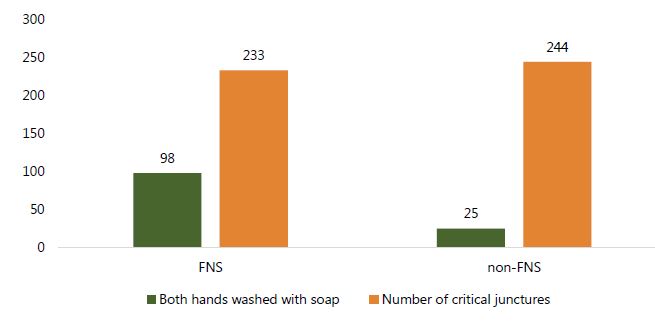
Table 7 summarizes data on critical junctures that occurred during the observation among all members of the compound in both groups and the instances when both hands were washed with soap. In total, 491 observed instances occurred that required handwashing to minimize risk of illness (see also Figures 4 and 5). Overall, we found a marked difference in observed behavior between FNS and non-FNS for all instances other than after handling livestock, and the difference is statistically significant at the 95 percent confidence level for all variables except for children under five after using the toilet (p less than 0.10). Although the concept and practice of cleaning hands are not uncommon in the target population, there continues to be a statistically significant difference (p=.000) between FNS households (70 percent) and non-FNS (51 percent) attempts to wash hands with any method involving soap and/or water. However, the fact that 51 percent of the time, members of non-FNS households washed their hands supports the existence of handwashing as an accepted practice.
Table 7. Total Number of Observed Critical Junctures and Handwashing of Both Hands with Soap among ALL Members of the Compound (Including Mothers)
| Critical Juncture Observed | FNS Households (n=61) | non-FNS Households (n=59) | P-value,8 95% CI | ||||
|---|---|---|---|---|---|---|---|
| Number of Observations | Number of Times Both Hands Washed with Soap | Percentage of Time Both Hands Washed with Soap | Number of Observations | Number of Times Both Hands Washed with Soap | Percentage of Time Both Hands Washed with Soap | ||
| After mother using toilet | 8 | 6 | 75% | 16 | 1 | 6% | 0.001 |
| After other adult using toilet (not mother) | 9 | 3 | 33% | 13 | 0 | 0% | 0.042 |
| After child (under 5) using toilet* | 31 | 7 | 23% | 36 | 3 | 8% | 0.168 |
| After cleaning child following toilet use/disposing of stool | 34 | 21 | 62% | 48 | 11 | 23% | 0.000 |
| Before food preparation | 51 | 29 | 57% | 37 | 2 | 5% | 0.000 |
| Before feeding child | 52 | 16 | 31% | 47 | 3 | 6% | 0.002 |
| Before eating | 35 | 13 | 37% | 32 | 2 | 6% | 0.003 |
| After handling livestock | 13 | 3 | 23% | 15 | 3 | 20% | 1.000 |
| Totals | 233 | 98 | 42% | 244 | 25 | 10% | 0.00 |
*Includes child washing own hands, someone else washing child’s hands, or having a bath.
Our data suggest that, in the absence of handwashing promotion, people tend to wash both hands with soap more often after cleaning a child’s bottom or disposing of stool than at other critical junctures, although the practice of proper handwashing is not common overall, at 23 percent. Given this basis from which to compare, people who have been exposed to handwashing promotion appear to modify their behavior in all instances to include soap and washing both hands. This is a critical issue to include in handwashing promotion, as handwashing as a practice is fairly common, but washing both hands and using soap is not common. Additionally, among the FNS group, we found considerable variation in when people are more likely to wash both hands with soap and in who washes their hands. Mothers who have completed handwashing education are more than twice as likely to practice proper handwashing as other FNS household members. Thus, the mother’s ability to influence those in her household to wash their hands may be overestimated. In the interviews, mothers reported reluctance on the part of mothers-in-law to use the tippy tap and wash their hands more often.
Proper handwashing is more frequent before food preparation than before eating or feeding a child, highlighting the need for more emphasis on clean hands for all handling of food. The difference may be partially explained by the custom of mothers (i.e., those who have received handwashing education) preparing the food while other family members may actually feed the child, again indicating that mothers may lack sufficient power in the household to influence behavior; and mothers are not the only potential vectors for disease transmission on the compound.
Figure 4. Handwashing practices observed at critical junctures among ALL members of a compound
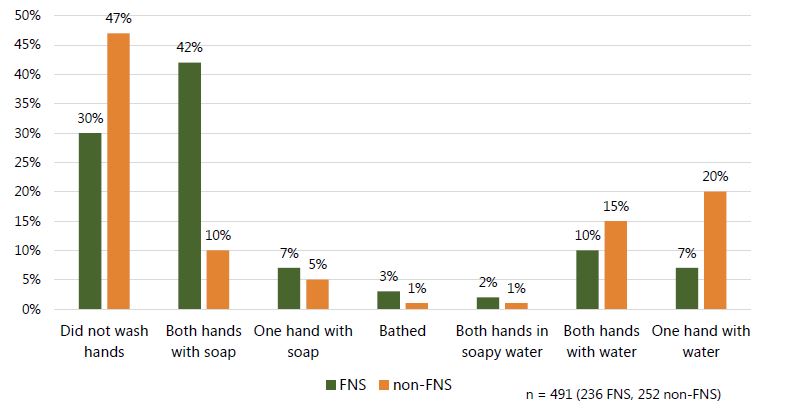
Figure 5. Percentage of times both hands were washed with soap by critical juncture among ALL members of a compound
Handwashing with Tippy Taps
In all 61 households of the observed FNS group, tippy taps were installed and used by all family members, and even neighbors. Mothers used tippy taps the most, but all household members were found to use them on occasion (See Figure 5). At 39 percent, husbands comprised the largest proportion of persons using the tippy tap other than the mother (n=37).
Figure 6. Tippy tap use among others present at the homestead (excluding mothers)
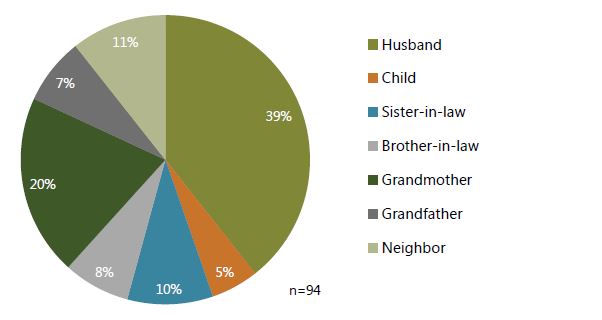
In 168 instances of handwashing observed in FNS households, the tippy taps were the most popular handwashing stations. A total of 77 of 139 mothers used the tippy taps to wash hands, and 16 of 29 other family members did so (Figure 6).
Figure 7. Most utilized sources of water for any handwashing among members of the FNS group at critical junctures9
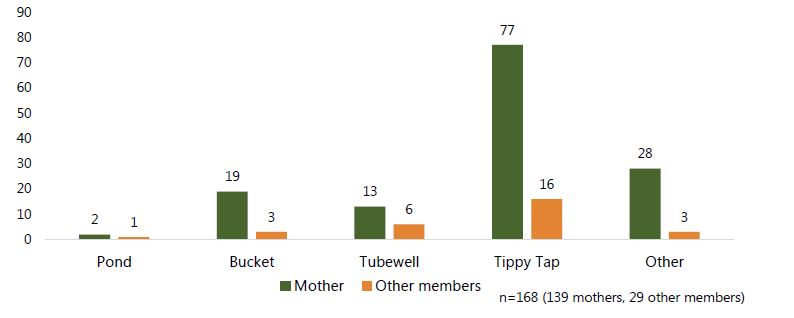
When both hands were washed with soap at critical junctures, all members of the FNS group were more likely to choose a tippy tap as a handwashing station. In fact, the FNS group used tippy taps 100 percent of the time for washing hands (when hands were washed) after using the toilet, and before eating (Figure 7).
Figure 8. Number of times both hands were washed with soap using the tippy tap among ALL members of FNS group at critical junctures
*Refers to both a child under five and a school-age child washing his/her own hands after going to the toilet
While about 60 percent (n=35) of non-FNS have their handwashing stations elsewhere on the premises, more than 90 percent (n=55) of FNS participants have their stations near the two strategic locations that we promote for handwashing: near the kitchen and near the latrine. “The kitchen and latrine are the places where we get dirty the most,” said an FNS respondent in. “I chose these locations for handwashing stations so that we can wash our hands immediately after getting dirty.”
Findings from Interviews
Self-Reported Knowledge and Attitudes toward Hygiene and Handwashing
In addition to observations, data collectors interviewed mothers from both groups (FNS=61, non-FNS=59) about their hygiene knowledge and practices, as well as the key informants.
Findings from the interviews and information provided by the key informants indicate that understanding of the link between contaminated hands and diseases has been incorporated into traditional beliefs about illness causation based in humoral theory.10 Respondents attributed illnesses equally to hot weather and excessive exposure to water as to “dirt” (e.g., being dirty). When asked, “What do you think was the reason your child got sick?” 27 percent of all women (n=32; 21 FNS, 11 non-FNS) cited dirt, 27 percent (n=32; 19 FNS and 13 non-FNS) listed water (usually excessive bathing or rainfall), and 23 percent (n=27; 15 FNS and 11 non-FNS) blamed hot weather. Hot weather and water appear to be related because hot weather causes people to sweat (i.e., water on the body) and motivates people to take more baths. Many women believe that more than one cause could result in illness; thus, many respondents had multiple answers, such as playing in the dirt and taking too many baths. FNS participants responded with one or more of these three causal factors more frequently than the non-FNS group, while more non-FNS women either had no response or gave other reasons. Furthermore, 10 percent of women (n=11) interviewed listed breastfeeding under pathogenic circumstances as a reason for illness, such as when the mothers themselves were sick, or the mother breastfed when she had been exposed to hot weather, or even after she had taken too many baths. “I was working in hot weather, then I breastfed my daughter right after coming back from that hot weather. I think this is the reason my child had diarrhea,” reported one non-FNS respondent in Boroitala village. Other illness causal factors mentioned include supernatural events (e.g., black magic) and bad food.
In addition to having a disease etiology based in both germ theory and humoral theory, respondents may not perceive “dirty hands” as a cause of acute respiratory infection (ARI) or fevers. When asked what illnesses are caused by dirty hands, an overwhelming majority (99 percent) of respondents named diarrhea; however, only five people (4 percent) said respiratory illness and 10 (8 percent) said fever. This finding should inform the approach to modifying practices among target groups. Messaging needs to emphasize the link between handwashing and all communicable illnesses, including fevers and ARI, in addition to the importance of proper handwashing at all critical junctures.
Our findings suggest that, in general, people may believe that if they do not actually see dirt on their hands, the hands are clean. Our Senior Technical Officer Nutrition at the Barisal office provided insight into this idea, stating that people in Barisal communities believe water is the main source of diseases. Our observations support this interview finding, with people less likely to wash their hands before handling food than at other times, thereby increasing risks of contamination of the food. In interviews, mothers identified water as a primary source of disease and illness, although this idea seemed to be situated within humoral theory and the pathology of excessive bathing or exposure to water rather than the context of water-borne illnesses. In response to the question “Why is handwashing important?” most respondents (46 FNS, 75 percent and 38 non-FNS, 64 percent) said that it kills germs and keeps them (40 FNS, 25 percent, and 35 non-FNS, 22 percent) and their babies (18 FNS, 11 percent, and 14 non-FNS, 9 percent) healthy. Other popular responses were that hands feel fresh (23 FNS and 18 non-FNS), and that handwashing prevents diarrhea (25 FNS and 20 non-FNS). We found no significant difference in responses between the two groups.
Almost all women (95 percent, no significant difference between the two groups) knew that the most effective way to wash hands is with soap and water. Within the FNS group, 62 percent (n=38) responded that the best way to clean hands is with soap and, specifically, water running from a tippy tap. More than 99 percent (n=119) of all respondents said that dirty hands can cause diarrhea when asked what kind of illness can be caused by dirty hands. However, only 40 percent (n=48) of all respondents cited washing children’s hands with soap as a way to prevent diarrhea, although more than double the number of FNS respondents (n=34, 56 percent) versus non-FNS (n=14, 24 percent) provided this response (p=0.001). In contrast, in the observations, participants in both groups did not wash children’s hands often, even after the child used the toilet.
The youngest child of approximately one-half of all respondents was reported to be affected by some kind of illness in the two weeks prior to the interview. Mothers mostly reported that their child had cough and fever, and sometimes diarrhea. However, mothers from the FNS group (n=4) reported their children to have had fewer incidences of diarrhea than non-FNS children (n=9). Additionally, children from the FNS group had diarrhea an average of three days, whereas non-FNS children suffered from diarrhea an average of four days. Although the sample size requires caution against overstating these findings, the data do indicate a possible trend.
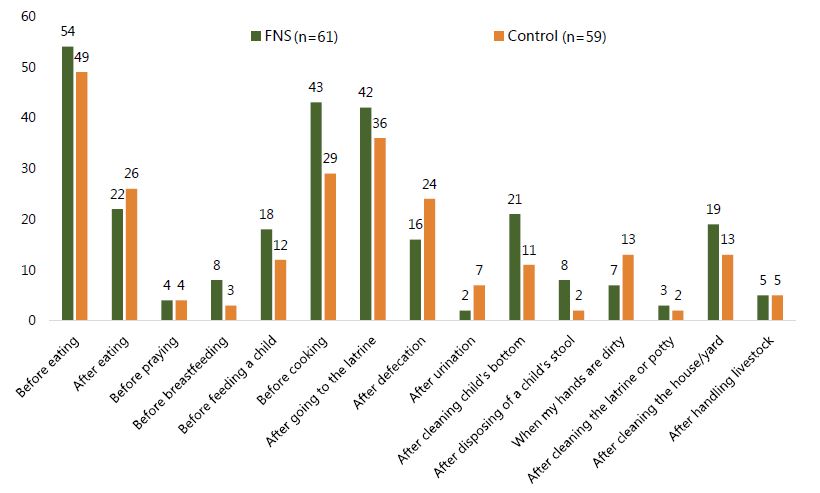
Overall, mothers in the FNS group had better knowledge on the critical times for washing hands, although there was greater agreement on some critical junctures than others (See Figure 8). A similar majority of FNS (89 percent, n=54) and non-FNS (83 percent, n=49) mothers said that it is important to wash hands before eating; however, a considerable gap between knowledge and observed behavior presents in the data, with only 21 percent of FNS mothers observed washing both hands with soap before eating and 26 percent before feeding a child. A majority of FNS mothers also believe it is important to wash hands before cooking (71 percent, n=43) and after using the latrine (69 percent, n=42). In contrast, while non-FNS respondents also share the knowledge that handwashing is important after using the latrine (61 percent, n=36), just under one-half think it is important before cooking (49 percent, n=29). We found a significant difference between the two groups in the number of people who said that washing hands is important before cooking (p=0.017). However, as previously stated, a gap persists between what mothers know and what they do.
Figure 9. Important times for handwashing reported by mothers from FNS and non-FNS groups
Overall, FNS mothers had better knowledge than non-FNS mothers of appropriate handwashing techniques, such as using soap, rubbing hands, washing between fingers, washing both sides of the hands, cleaning the nails, rinsing with clean water, and drying hands (approximately 60 percent vs. 40 percent). However, this difference was not statistically significant between the two groups.
Generally, mothers from the FNS group felt satisfied with their current handwashing practices, whereas about one-quarter of the non-FNS group respondents were not happy with their handwashing. One of the reasons was unavailability of clean water. “The tubewell is far away from my house. So, tubewell water is not available for us to wash [our] hands,” said a non-FNS respondent in Rangasree.
Interviewers asked the participants why they chose the location of their current handwashing station. Table 8 shows the most popular reasons. As the table indicates, FNS participants overwhelmingly choose to have a handwashing station specifically near the latrine or kitchen, compared to non-FNS participants. In fact, only five non-FNS participants put a handwashing station near the latrine. It is important to remember that these participants do not use a tippy tap, but usually the tubewell, which may not be near the latrine and, thus, not in a location that supports proper handwashing at critical junctures.
Table 8. Reason for Preferred Handwashing Station Location by Number of Respondents Citing Each Reason (Percentage)
| Why did you choose this location for your handwashing station? | FNS (n=61) | Non-FNS (n=59) |
|---|---|---|
| It is convenient | 37 (61%) | 28 (48%) |
| It is close to my kitchen | 34 (56%) | 16 (27%) |
| I can quickly go to it | 27 (44%) | 17 (29%) |
| It is close to my latrine | 30 (49%) | 5 (9%) |
Among non-FNS group respondents, some (n=12, 20 percent) recognized that, in order to wash their hands with soap more frequently, they need some kind of device that can hold water, and it needs to be located where handwashing should take place. However, 15 mothers (25 percent) from the non-FNS group also said that, without a tubewell nearby, it may be hard to improve handwashing behavior. The significant difference in handwashing behavior found between households where a tubewell is visible from the kitchen or latrine and households where a tubewell is not visible from the kitchen or latrine supports this claim. Furthermore, priority may be given to certain handwashing junctures if water is not readily available to wash hands at all such junctures.
Interviewers asked participants whether or not anyone had ever criticized them for washing their hands with soap. Almost 12 percent of all women answered affirmatively to this question. Although reported criticism was low, more non-FNS than FNS participants (4 FNS vs. 10 non-FNS) reported being criticized by elders (e.g., mothers-in-law) or neighbors. The following quotes illustrate the criticism faced by some mothers:
Some people who are not good, they taunt me and keep saying, see, [you] cannot afford to eat regularly but [you] wash hands with soap. But I don't care because I know how important it is.
—FNS respondent, Dibuapur
They laugh at me, they think I am showing off my cleanliness.
—non-FNS respondent, Katenga
They ask me ‘Why do you wash your hands so many times?’
—FNS respondent, Barakpur
Self-Reported Attitudes Toward Tippy Taps
This section of the report contains only responses from FNS participants since only members of the FNS group had tippy taps installed at their compounds.
The use of tippy taps has been widely adopted in communities who received FNS training, with sixty-two percent of the population now using tippy taps regularly. The knowledge about the importance of handwashing motivates them to keep using it. Before installing a tippy tap, respondents used a tubewell (52 percent, n=32), pond (31 percent, n=19), or bucket/pitcher (37 percent, n=23) for handwashing.
Seventy-nine percent (n=48) said they have to refill their tippy tap once or twice a day, indicating frequent use of their device. Observers noted no difference between FNS and non-FNS in the number of women who retrieved water during the observation (72 percent FNS and 69 percent non-FNS). However, during the observation, we noticed that rather than using 1- or 2-liter bottles for construction of the tippy tap, many households had small, 0.25-liter bottles. To the question as to how often their tippy tap needs to be repaired, women said almost never, although sometimes tying it tighter to the tree was required. While no consistent answer emerged as to how many times the bottle for the tippy tap needed to be replaced, the most popular answers were one to three times per month (49 percent, n=30), or at least once after about six months of use (38 percent, n=23). Respondents did mention that the time the bottle lasts depends on the quality.
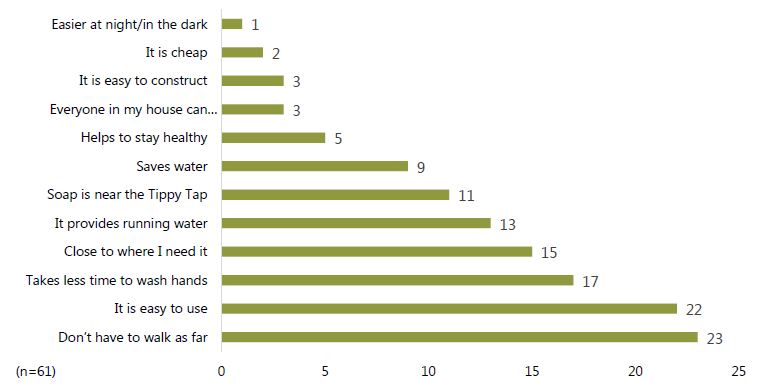
When asked “Why did you decide to install a tippy tap in your home?” the majority of FNS respondents said it is easy to use. Other common reasons were household members do not have to walk as far to wash hands, it is close to where it is needed, it does not need a lot of water, it takes less time to wash hands, and all family members can use it. (Table 9 shows all responses.)
Table 9. Reason Given for Installing a Tippy Tap
| Why did you decide to install a tippy tap in your home? | FNS11 (Percentage) |
|---|---|
| Easy to use | 34 (56%) |
| Do not have to walk as far to wash hands | 18 (30%) |
| Close to where I need it | 17 (28%) |
| Does not need a lot of water | 16 (26%) |
| Takes less time to wash hands | 15 (25%) |
| All members of the family can use it | 12 (20%) |
| To be clean and healthy | 10 (16%) |
| Because I was told to | 5 (8%) |
| Soap is near it | 5 (8%) |
| Keeps water safe and clean from contamination | 3 (5%) |
| Easy to construct | 2 (3%) |
| Cheap | 2 (3%) |
Forty-two respondents (69 percent) said that their children also use tippy taps for handwashing. However, some mothers (21 percent, n=13) said that their children use the tippy tap a toy. The children sometimes let the water run out, break it, or take it down. Our Senior Technical Officer Nutrition at the Barisal office added that mothers frequently report that children exchange the bottles used for tippy taps with street vendors for sweets (the vendors then sell the bottles to a processing plant for money). One interviewed mother relayed a similar experience. “Once my two little brothers sold the bottle to buy ice cream. But they use it and often they fill the Tippy Tap with water from the tubewell,” said an FNS respondent in Nobipur.
Women said that their husbands generally support the use of tippy taps. Forty-six men (75 percent of husbands) were reported by their wives to use them for handwashing as well, while only 23 mothers-in-law expressed an interest in using a tippy tap.
Since installing a tippy tap, respondents reported a number of positive changes. The biggest change in the lives of the FNS participants is a marked increase in frequency of handwashing. Seventy-one percent (n=41) say they wash their hands more frequently now that they have a tippy tap. Other changes include washing hands before preparing food and before eating, a healthier family, and simply remembering to wash hands. Figure 9 displays these changes and the number of participants reporting them.
Figure 10. Reported changes since installing a tippy tap12
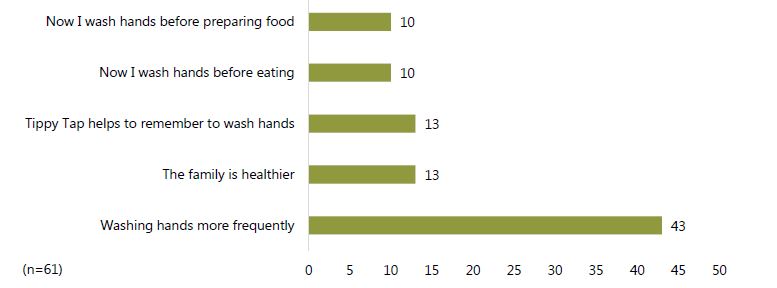
It is unclear, however, whether these changes result purely from the presence of a tippy tap in the household. Most likely, they stem from a combination of the promotion of tippy taps and overall handwashing education from our SPRING facilitators and extension health workers, since all mothers in the FNS group also completed such education. Although approximately 70 percent of women in the FNS group reported that they started washing hands more frequently, only about 21 percent said that their family is healthier. Possibly, not enough time has passed for them to notice the difference in health outcomes, or perhaps other family members do not use the tippy taps as frequently as the mothers. Other family members were observed using the tippy taps less frequently. These family members could continue to transmit disease with contaminated hands.
When asked what they think about tippy taps, all (n=61) respondents gave positive answers, such as it is good, easy to use, or convenient. The quotes below are illustrative of the responses:
I want to keep it up. I will never give up this practice [using a tippy tap.]
—FNS respondent, Parukhali
It is good for me. Because we can keep away from diseases, and if I am in a hurry, I can wash hands quickly with a tippy tap without going to the pond.
—FNS respondent, Pascim Charpata
It takes less water. Close to where I need. It inspires us to wash hands.
—FNS respondent, Parukhali
Seventy-nine percent (n=48) of FNS participants said that either people asked them about the tippy tap or they promoted it to their friends and neighbors. “I asked Rahima about the use of a tippy tap when I did not have one. After using it, now I am talking about the advantage of it with my sister-in-law,” reported one FNS respondent in Kochabunia.
Key informants (Community Health Care Provider, Health Assistant, and an FNS leader), interviewed stated that villagers are impressed by the simple technology of the tippy tap. Indeed, one key informant said, “Neighbors were impressed with its mechanism. Water starts pouring when air enters the bottle after unscrewing the cap…That impressed them and many of them asked about it. I told them and also told my relatives about its benefits. Some of them are using it now.”
The majority of women said their relatives and neighbors want to learn what a tippy tap is and what its benefits are. “At first, my sister-in-law was laughing at me to see this, but later she asked me to show her how to make it,” said an FNS respondent in Pascim Charpata. A woman from Dibuapur said, “Many of my neighbors and relatives are also interested to know about tippy taps. Interestingly, a couple of days ago my nephew came to visit me and he saw my tippy tap. After coming back home, he insisted that his mother make one for him.” However, acceptance and interest are not unanimous. One woman from Nobipur said, “Some people asked me about a tippy tap. Some use it and some do not, but generally people of our village do not care about it.”
A majority of all FNS participants (n=58) reported no challenges associated with using a tippy tap. Of the three women who did mention challenges, two said soap is expensive or a bottle is unavailable.
Respondents gave various reasons for liking tippy taps, such as it “helps to stay healthy” and it “saves water.” However, the most popular answers were: “[You] don’t have to walk as far” (38 percent, n=23) and “It is easy to use” (36 percent, n=22). Figure 10 displays all reasons given by FNS respondents.
Figure 10. Reasons FNS participants like their tippy taps13
For many women, the novelty of the tippy tap was a significant attraction. “It is like an automatic tap, which we can see in the city. So, I feel good to use it,” said an FNS respondent from Pascim Charpata. A woman from Kelashpura village told the interviewer, “Water falls from a tippy tap like from a real tap. We have never seen it before, so I like it.”
While most women (87 percent, n=53) had nothing negative to report about a tippy tap, a few (7 percent, n=4) said that they did not like refilling it too often. One person did not like that it takes too long to wash her hands.
Almost one-half of FNS participants express satisfaction with the design of the tippy tap. However, while responding to the question about changes that would make the tippy tap more useful, 25 women (41 percent) said that a bigger bottle would be better. Additional suggestions are as follows:
If I can keep a tippy tap inside the house, then it will be nice. During the rainy season it is hard to wash [your] hands if I have to go outside.
—FNS respondent, Motherbunia
If it had a long pipe system then it would be very easy to use. If it had a big container, then I would not have to refill it frequently.
—FNS respondent, Fokrunnessa, Kochabaria
I want to follow SPRING. SPRING taught me about washing hands and about using tippy tap, and now I am using it. If SPRING brings any changes I will adopt them.
—FNS respondent, Shahnaz, Nachuniya
Discussion and Recommendations
Discussion
Our study provides strong evidence of the acceptability and effectiveness of tippy taps as well as hygiene and sanitation education in 10 upazilas of the Barisal and Khulna divisions of Bangladesh. All households in which women had attended a SPRING FNS had a tippy tap installed, whereas no households included in the study that had not attended a SPRING FNS had a tippy tap. In the FNS group, 93 percent of households had two tippy taps installed, usually one by the latrine and one near the kitchen, and several had three or more.
In general, we found better handwashing knowledge and practices in the FNS group than in the non-FNS group. For example, structured observations indicated that handwashing in general and washing both hands with soap were more common at all critical junctures in the FNS group. In a majority of cases (55 percent) when FNS household members washed hands, they used tippy taps, while the most common handwashing stations for non-FNS participants were buckets and tubewells.
Interviews with mothers indicated greater knowledge on handwashing in the FNS group than in the non-FNS group. Of 15 possible moments where handwashing would be beneficial, nine were mentioned more frequently by FNS respondents than by the non-FNS group, while only four were mentioned more often by the non-FNS group. The FNS group also indicated greater understanding of the link between washing hands and preventing diarrhea. In addition, our study found high acceptability among tippy tap users, with respondents commenting that it makes handwashing easier and more convenient, resulting in more frequent washing.
When taken together, information from the various sources suggests that the first question our study sought to answer may be answered affirmatively and with confidence. That question was:
Does the presence of tippy taps improve handwashing practices at critical junctures and among different members of the same household, where one member (pregnant or lactating woman/mother of child under two) recently received information on handwashing and has agreed to set up a tippy tap in the household?
Results from the observations clearly illustrate better practices in FNS households, with other members (i.e., not the mother) in FNS households exhibiting proper handwashing behavior in 42 percent of instances, compared to only 10 percent of such instances in non-FNS households. However, in the interviews, mothers reported their husbands to be more accepting of the tippy tap than their mothers-in-law.
Our second study question was:
Does the presence of the tippy tap near the kitchen improve handwashing practices prior to handling food, eating, and feeding a child?
This was not explicitly answered, because our analysis did not distinguish between use of the kitchen tippy tap and other tippy tap(s), although the fact that 59 of 61 households in the FNS group had tippy taps in the kitchen suggests that the positive results reported for handwashing prior to handling food, eating, and feeding the child can most likely be attributed to the kitchen tippy tap. In that case, we see that washing both hands with soap before those three critical moments was significantly more likely in the FNS groups than the non-FNS group, suggesting that a kitchen-based tippy tap does encourage improved handwashing practices.
Despite these impressive findings, much room for improvement remains in several areas. For example, although we found notable improvements in knowledge and practices in the FNS group, both knowledge and practices remain weak in many areas. Even in the FNS group, women washed both hands with soap in fewer than one-half of all potential critical handwashing moments, and only in two of those junctures (after using the toilet and after disposing of stool) did handwashing occur 75 percent of the time or more. We also identified knowledge gaps in both groups, especially with relation to the connection between contaminated hands and disease. While most FNS respondents attribute dirty hands to diarrhea, few make the same connection to ARIs and fevers. Furthermore, there may be a tendency to think hands are not dirty in the absence of visible dirt. ARIs and fevers are more likely to be attributed to water and heat as part of a broader disease etiology based in humoral theory.
Finally, although our study strongly suggests that tippy taps can improve handwashing practices, other water and sanitation issues also affect health, and these should be addressed in addition to tippy tap interventions. For example, observers found that stool was present on the ground in a large majority of compounds in both groups. In most cases this was animal stool, but in 5 percent of households, human stool was present as well, and observers noted 35 instances of children defecating on the ground. A greater impact on hygiene and health will be more likely in the context of addressing broader sanitation issues as part of handwashing education, along with tippy tap promotion and use.
Recommendations for Future Actions
During FNS, health facility, and community gatherings:
- Promote placing multiple tippy taps in convenient locations for the household to address all the convenience concerns. Include messages on the convenience of using tippy taps.
- Include messages on the practice of keeping the compound clear of animal and human feces. SPRING has already begun placing greater emphasis on handwashing after touching or being in contact with animals and raised biosecurity as a more prominent component of its community-level work.
- Include messages on the practice of disposal of child’s feces in latrines, highlighting that children’s feces also carry germs.
- Include messages on the practices of washing the young child’s hands frequently throughout the day, as children are likely touch the ground and put their hands in their mouths.
- Emphasize practices of handwashing after handling livestock and before food preparation or eating.
- Emphasize the importance of handwashing of all family members/caregivers before taking care of the child, especially before feeding the child.
- Consider including information about the challenges associated with the use of tippy taps, such as children exchanging the bottles for sweets during FNS sessions. Beneficiaries can be given different scenarios and advised on the ways to better deal with such situations.
- Provide communication support through a union authority, such as a government circular or public announcement, to address issue for all, not only women and children.
- Emphasize the link between handwashing and all diseases (e.g., ARIs and fevers), and explain the connection between germs and nutritional status of children. Educators can do this through games and other activities that explain how invisible germs get transferred from one person to another or from a contaminated surface to a person through touching.
- Promote the use of bigger bottles (or larger containers) for tippy taps, especially in geographic areas where tubewells are less common.
- Include activities targeting non-FNS households in the surrounding areas to have a tippy tap installed, potentially equipping FNS members with messages to teach non-FNS households about tippy tap use and hand hygiene.
Footnotes
1 In this study, all critical junctures included mother using the toilet, another adult/caregiver using the toilet, children using the toilet, caregiver cleaning child’s bottom after defecation, caregiver disposing of child’s stool, before food preparation, before feeding a child, before eating, and after handling livestock.
2 Other handwashing stations/methods include a bucket, which may be filled with pond water or tubewell water, accompanied by a small handheld pitcher for pouring (note: only the right hand will hold the pitcher, and therefore, typically, only the left hand is washed in this manner); washing hands directly in the pond; washing hands at the tubewell by pumping the water and then washing in the stream (note: both hands can be washed at one time, but the right hand will be used to pump the water initially).
3 Recent” means that the FNS members graduated from the FNS in the previous year.
4 Due to unavailability or refusal to participate, nine randomly chosen participants had to be replaced by alternates in order to accomplish the planned 120 observations and interviews. In one case, the switch was made incorrectly, when a woman from the non-FNS group was switched for the FNS group. This resulted in 61 in the FNS group and 59 in the non-FNS group.
5 All critical junctures included in this observation are mother using the toilet, another adult using the toilet, child using the toilet, caregiver cleaning child after defecation, caregiver disposing of child’s stool, before food preparation, before feeding child, before eating, and after handling livestock.
6 In this case, any type of handwashing behavior was noted, such as one hand without soap, both hands without soap, one hand with soap, both hands with soap, both hands in soapy water, and bathing.
7 “Other” sources included river, water on a plate, and uncertain sources.
8 Based on Fisher’s test for all indicators with cell values >5 (otherwise, chi-square test).
9 “Other” sources included river, water on a plate, and uncertain sources.
10 “Humoral theory was one of the central principles in Western medicine from antiquity through the 19th century. The human body was thought to contain a mix of the four humors (or fluids): black bile (also known as melancholy), yellow or red bile, blood, and phlegm. Each individual had a particular humoral makeup, or “constitution,” and health was defined as the proper humoral balance for that individual. An imbalance of the humors resulted in disease.” (The President and Fellows of Harvard College 2015)
11 Multiple answers were allowed.
12 Multiple responses were allowed.
13 Multiple responses were allowed.
References
Biran, A. 2011. Enabling Technologies for Handwashing with Soap: A Case Study on the Tippy-Tap in Uganda. Washington, DC: Water and Sanitation Program.
Canadian Paediatric Society. 2001. “Handwashing for Parents and Kids.” Paediatrics & Child Health 6(1):53–54.
Global Public-Private Partnership for Handwashing with Soap (PPPHW). 2013. “Why Handwashing?” Accessed September 24, 2015, http://globalhandwashing.org/why
Gracey, M. 1996. “Diarrhea and Malnutrition: A Challenge for Pediatricians.” Journal of Pediatric Gastroenterology & Nutrition 22(1):6–16.
Hernandez, O., D. Jacqueline, J. Karver, C. Chase, and Y. Coombes. 2012. Measuring the Behavioral Determinants of Handwashing with Soap. Washington, DC: Water and Sanitation Program.
Humphrey, J. H. 2009. “Child Undernutrition, Tropical Enteropathy, Toilets, and Handwashing.” Lancet 374:1032–1035.
Icddr, B. 2012. “Uptake of Handwashing with Soap or Soapy Water from a Large-scale Cluster Randomized Community Trial in Urban Bangladesh.” Health and Science Bulletin 10(4):9–15.
The Joint Commission. 2009. Measuring Hand Hygiene Adherence: Overcoming the Challenges. Oakbrook Terrace, IL: The Joint Commission.
Luby, S. P., A. K. Halder, T. Huda, L. Unicomb, and R. B. Johnson. 2011. “The Effect of Handwashing at Recommended Times with Water Alone and with Soap on Child Diarrhea in Rural Bangladesh: An Observational Study.” PLoS Med 8(6):e1001052.
Ngure, F. M., B. M. Reid, J. H. Humphrey, M. N. Mbuya, G. Pelto, and R. J. Stoltzfus. 2014. “Water, Sanitation, and Hygiene (WASH), Environmental Enteropathy, Nutrition, and Early Child Development: Making the Links.” Annals of the New York Academy of Sciences 1308:118–128.
The President and Fellows of Harvard College. 2015. Contagion: Historical Views of Diseases and Epidemiology. Humoral Theory. Harvard University Library Online. http://ocp.hul.harvard.edu/contagion/humoraltheory.html
Rabbi, S. E., and N. C. Dey. 2013. “Exploring the Gap between Hand Washing Knowledge and Practices in Bangladesh: A Cross-sectional Comparative Study.” BMC Public Health 13:89.
Schreyer Honors College. 2014. “10 Questions: Ce Zhang.” http://www.shc.psu.edu/students/interviews/zhang.cfm
Solomons, N. W., M. Mazariegos, K. H. Brown, and K. Klasing. 1993. “The Underprivileged, Developing Country Child: Environmental Contamination and Growth Failure Revisited.” Nutrition Reviews 51:327–332.
U.S. Agency for International Development (USAID). 2013. Integrating Water, Sanitation, and Hygiene into Nutrition Programming. Washington, DC: USAID.